Abstract
Background: Diffuse large B-cell lymphomas (DLBCLs) with MYC -rearrangement (MYC -R) or double protein expression (DE) of the MYC and BCL2 are associated with poor prognosis. MYC -R reportedly occurs in approximately 5-14% of DLBCL cases. While the pathological and genetic prognostic factors for DLBCL with MYC -R have been reported, the clinical prognostic factors, including the extranodal sites involved, have not been fully elucidated. In the updated National Comprehensive Cancer Network guidelines for non-Hodgkin lymphomas, the presence of pleural effusion is a poor prognostic criterion for low-grade B-cell lymphomas; however, its prognostic significance in high-grade B-cell lymphomas is unclear. Therefore, we aimed to investigate the association between the presence of pleural effusion at diagnosis and outcomes in DLBCL with MYC -R or DE.
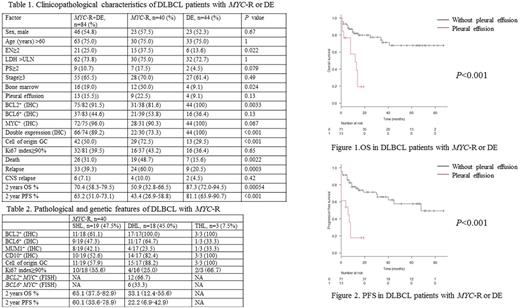
Methods: To explore the prognostic significance of pleural effusion in high-grade B-cell lymphoma, we assessed the medical records of DLBCL patients with MYC -R or DE, treated at the Juntendo University Hospital and Juntendo University Urayasu Hospital from December 2009 to June 2017. A total of 84 patients, including 40 with MYC -R and 44 with DE, were assessed. All patients were treated with R-CHOP-based regimens, with minor modifications. Rearrangements of MYC, BCL2, and BCL6 were detected using fluorescence in situ hybridization. The presence of pleural effusion at diagnosis was evaluated by using radiographic evidence from computed tomography and/or positron emission tomography-computed tomography. This study was approved by the Institutional Review Board of Juntendo University Hospital. We analyzed the relationships of overall survival (OS) and progression-free survival (PFS) with age, sex, lactate dehydrogenase (LDH) level, Eastern Cooperative Oncology Group performance status (PS), stage, the presence of ≥2 extranodal sites, pleural effusion, and bone marrow, peripheral blood, bone, gastrointestinal tract, lung, paranasal sinus, and skin involvement. Univariate and multivariate analyses of the estimated risk factors for OS and PFS were performed using the log-rank test and Cox proportional hazard regression analysis, respectively.
Results: The median age of the patients was 73 years (range: 39-92 years), 75% of the patients were older than 60 years, and 54.8% were male. Elevated LDH levels, PS ≥2, advanced stage disease, and ≥2 extranodal sites were found in 73.8%, 10.7%, 65.5%, and 25% of patients, respectively (Table 1). At diagnosis, pleural effusion was observed in 13 patients (15.5%; MYC -R: nine cases, DE: four cases). The presence of lymphoma-associated pleural effusion was confirmed on cytological evaluation in seven of these cases. The median OS and PFS was 14.5 (range: 1-87) and 13 (range: 0-87) months, respectively. Patients with pleural effusion at diagnosis had significantly shorter OS and PFS than those without pleural effusion (median OS: 8 months vs 18 months, P<0.001; median PFS: 4 months vs 15 months, P<0.001, Figure1 and 2). The multivariate analysis showed that pleural effusion (hazard ratio [HR] 3.2, 95% confidence interval [CI] 1.2-8.1, P=0.015) and bone marrow involvement (HR 3.1, 95% CI 1.2-7.7, P=0.015) were significantly associated with inferior OS. Pleural effusion (HR 4.3, 95% CI 1.6-12.1, P=0.0050) and PS ≥2 (HR 3.2, 95% CI 1.2-8.8, P=0.022) were significantly associated with inferior PFS.
Conclusions: The presence of pleural effusion at diagnosis was independently associated with inferior OS and PFS in DLBCL with MYC -R or DE. These results may significantly influence the clinical management of DLBCL patients with MYC -R or DE. Because the presence of pleural effusion at diagnosis is a high-risk factor, it should be routinely evaluated, especially in patients with high-grade B-cell lymphoma.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal